Burnout is no longer a buzzword—it’s a daily reality for many clinicians. For Nurse Practitioners (NPs) and Physician Assistants (PAs), the weight of full patient panels, endless inbox messages, and rising administrative demands can take a toll on both well-being and quality of care.At PsyPhyCare, we recognize that supporting practitioners goes beyond job placement. We want to equip you with strategies you can use to not just survive—but thrive—in today’s primary care environment.
The Anatomy of a Well-Run Practice
A low-burnout practice is one where clinicians experience:
- Time and connection with patients
- Manageable workloads
- Low administrative burden
- Teamwork and trust
- Support for individual well-being
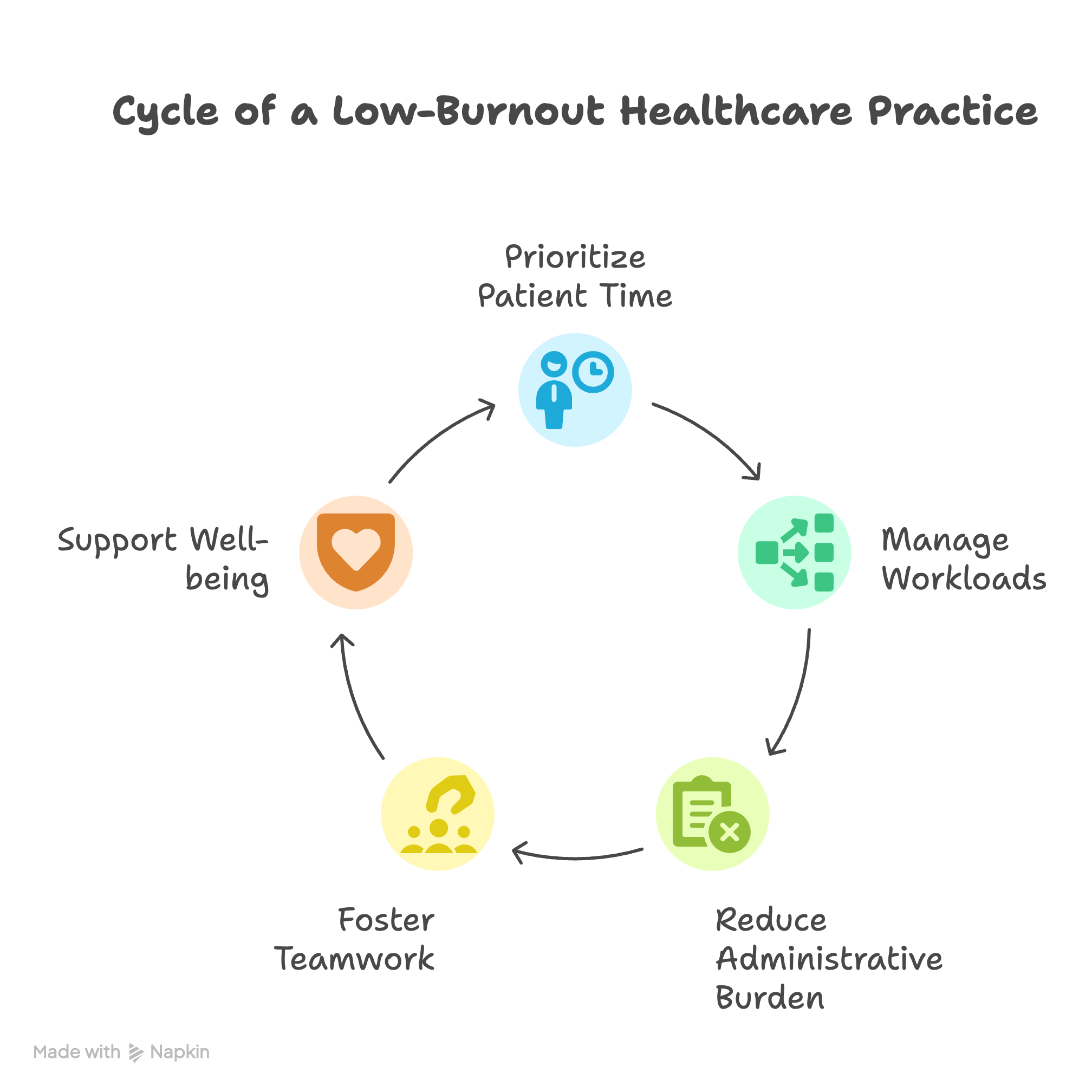
These conditions don’t happen by accident—they come from intentional changes at the system and individual level.
Three Strategies to Combat Burnout
1. Stop the Unnecessary Work
- De-implement low-value tasks: Push back on workflows that don’t improve patient outcomes. Identify tasks that consume significant time but contribute little to patient care or overall efficiency. This might involve questioning established protocols or advocating for changes in administrative procedures.
- Streamline documentation: Use smart phrases, templates, and coding toolkits to reduce “note bloat.” Standardize documentation processes to minimize repetitive typing and ensure that notes are concise and focused on essential information. Explore the use of voice recognition software to expedite documentation.
- Make portal messages count: Convert patient portal communications into billable encounters. Implement policies and procedures to appropriately bill for time spent addressing patient inquiries and providing medical advice through the patient portal, where applicable and compliant with regulations.
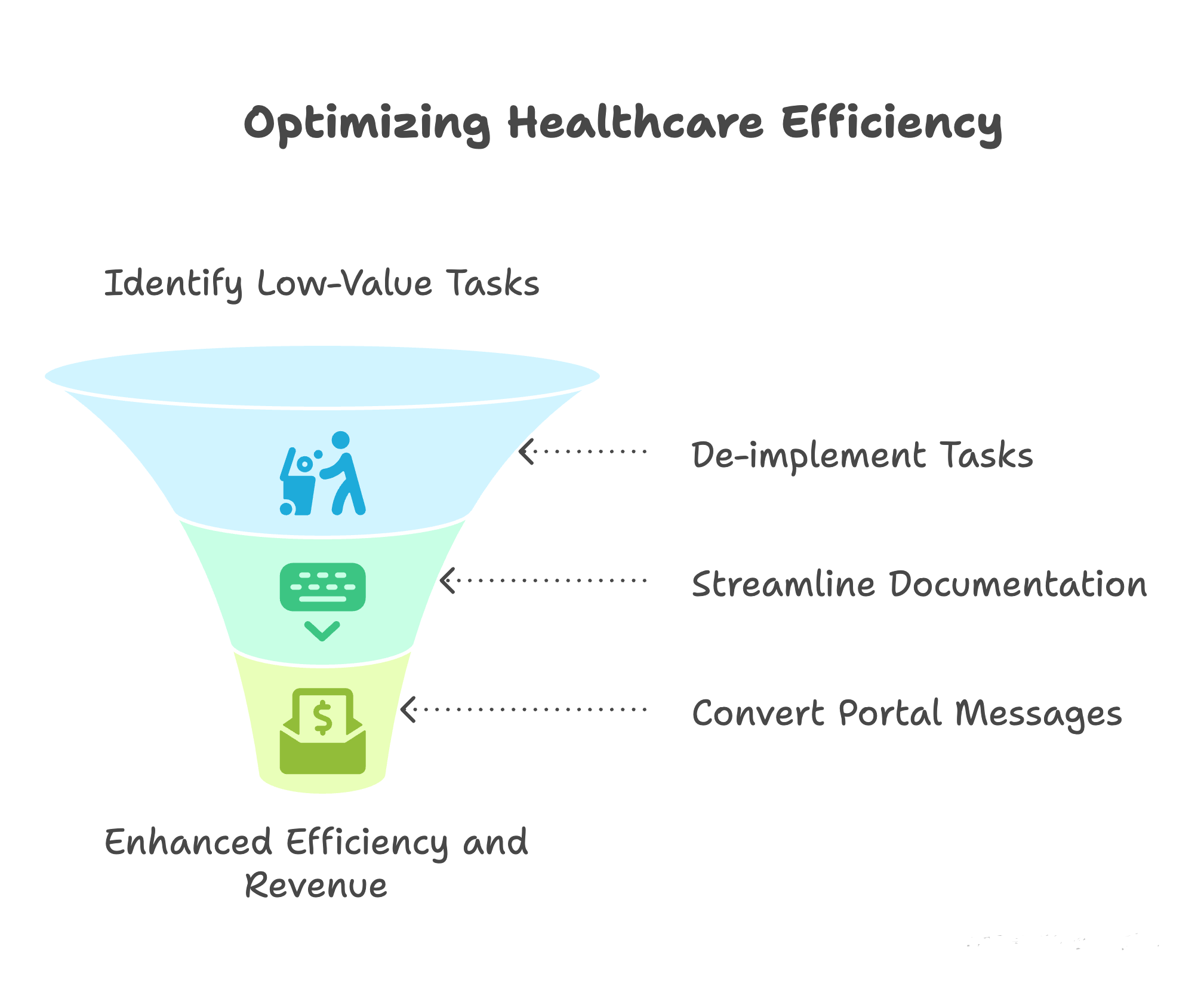
📌 Resource: AMA De-Implementation Checklist
2. Share the Necessary Work
- Team-based workflows: Lean on medical assistants or RNs for pre-visit planning, medication reconciliation, and documentation. Delegate tasks to other members of the healthcare team to optimize the use of each professional's skills and expertise. This can free up NPs and PAs to focus on more complex patient care activities.
- Inbox management: Develop shared responsibility for patient messages and lab results. Establish clear protocols for triaging and responding to patient messages and lab results, ensuring that these tasks are distributed among the healthcare team to prevent overload on individual clinicians.
- Annual prescriptions (“90x4”): Renew stable meds for a full year to avoid unnecessary refill requests. For patients with stable chronic conditions, consider prescribing medications for a full year (with appropriate refills) to reduce the frequency of refill requests and minimize administrative burden.
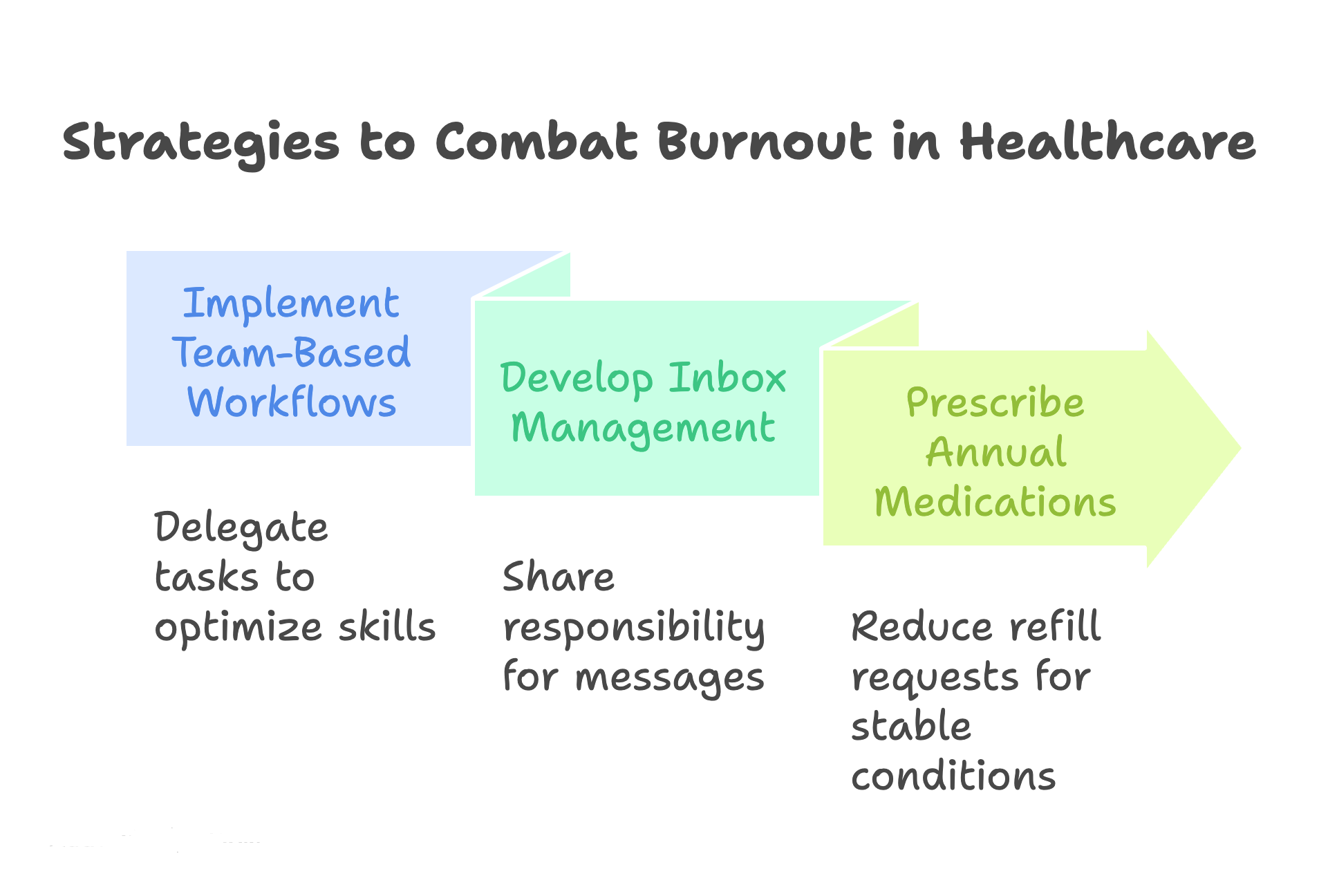
📌 Resource: AMA Team-Based Care Module
3. Support the Individual Clinician
- Schedule flexibility: Telehealth options and autonomy in daily schedules. Offer flexible scheduling options, including telehealth appointments and the ability for clinicians to manage their daily schedules to accommodate personal needs and preferences.
- Protected time: Ensure inbox coverage during vacations and PTO. Implement systems to ensure that patient inboxes are monitored and managed during clinician vacations and PTO, preventing a backlog of messages and reducing stress upon return.
- Peer support: Mentorship, professional development opportunities, and wellness workshops. Provide opportunities for mentorship, professional development, and wellness workshops to support clinician well-being and foster a sense of community.
- Value alignment: Open communication channels between clinicians and leadership. Foster open communication channels between clinicians and leadership to ensure that clinician concerns are heard and addressed, and that organizational values align with clinician well-being.
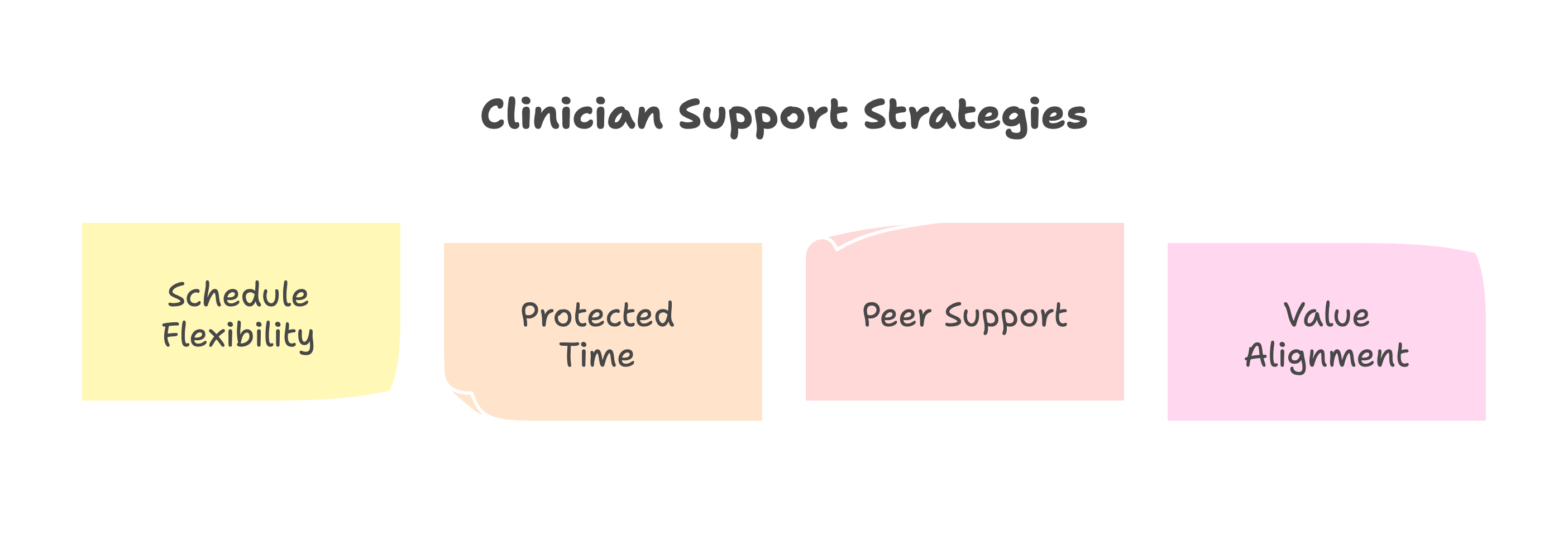
📌 Resource: AMA Clinician Well-Being Toolkit
What This Means for You as a Practitioner
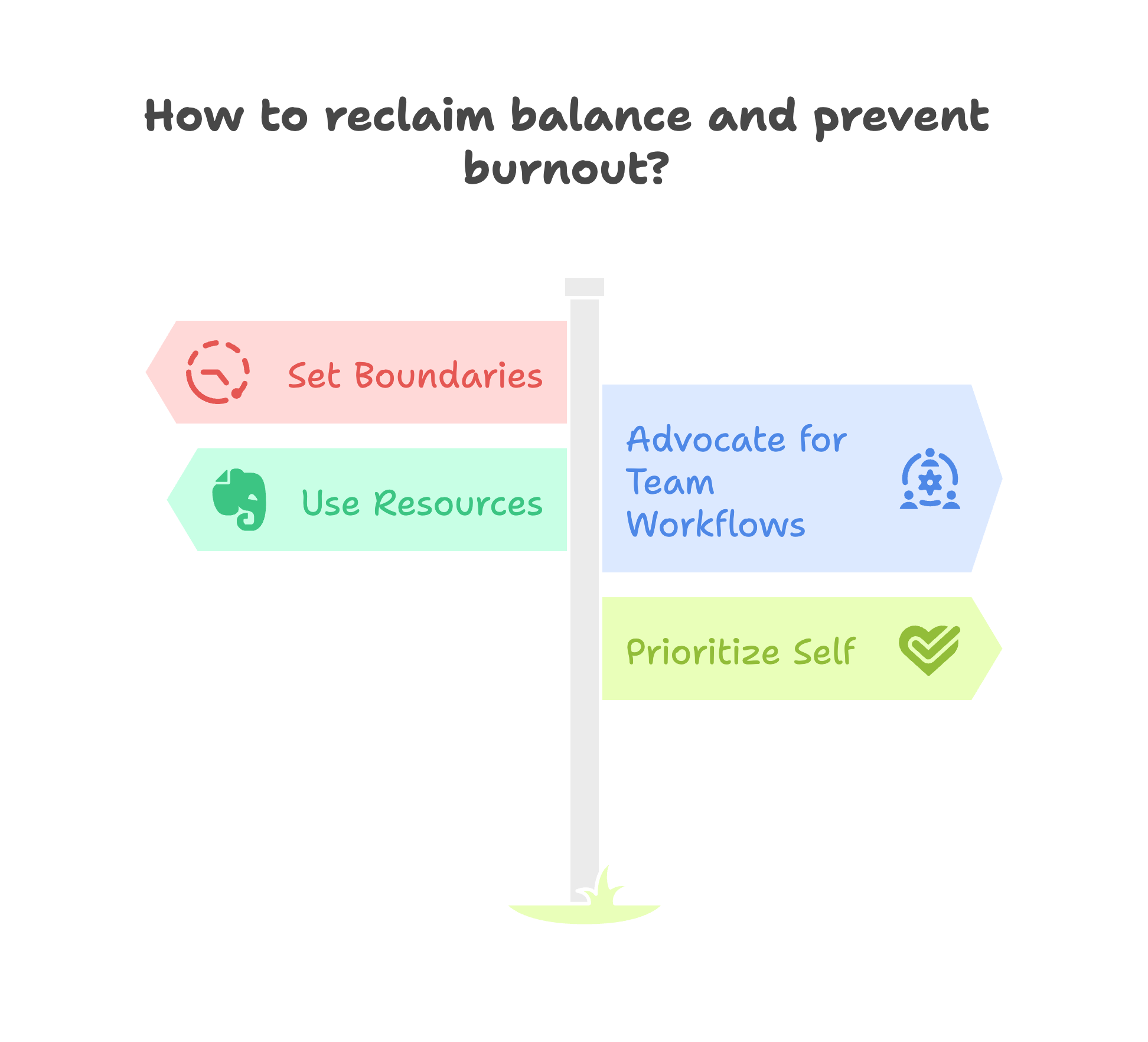
Burnout is not an individual failing—it’s a systems issue. But individual strategies can help you reclaim balance:
- Set boundaries with “free work” like after-hours charting. Establish clear boundaries between work and personal life, avoiding after-hours charting and other unpaid work activities.
- Advocate for team-based workflows in your practice. Actively advocate for the implementation of team-based workflows in your practice to distribute workload and improve efficiency.
- Use available resources—from AMA toolkits to mindfulness practices. Take advantage of available resources, such as AMA toolkits and mindfulness practices, to support your well-being and manage stress.
- Prioritize yourself—your patients thrive when you do. Recognize that prioritizing your own well-being is essential for providing high-quality patient care.
- Set boundaries with “free work” like after-hours charting.
- Advocate for team-based workflows in your practice.
- Use available resources—from AMA toolkits to mindfulness practices.
- Prioritize yourself—your patients thrive when you do.
Our Commitment at PsyPhyCare
We know that well-supported clinicians provide the best patient care. That’s why we:
- Connect you with organizations that prioritize wellness.
- Share resources that improve practice efficiency.
- Advocate for environments where professional & passionate practitioners can flourish.
Together, we can move beyond burnout and create healthcare systems that care for both patients and providers.
✨ Looking for more resources? Explore the AMA’s Steps Forward modules for practical strategies to enhance efficiency and well-being. https://edhub.ama-assn.org/steps-forward
"Insights adapted from Dr. Jill Jin’s presentation, Combating Clinician Burnout: Practical Strategies for Primary Care Practices, presented at Pri-Med Midwest 2024, and AMA Steps Forward resources"